Cervical Cancer- Symptoms, Causes and Treatment
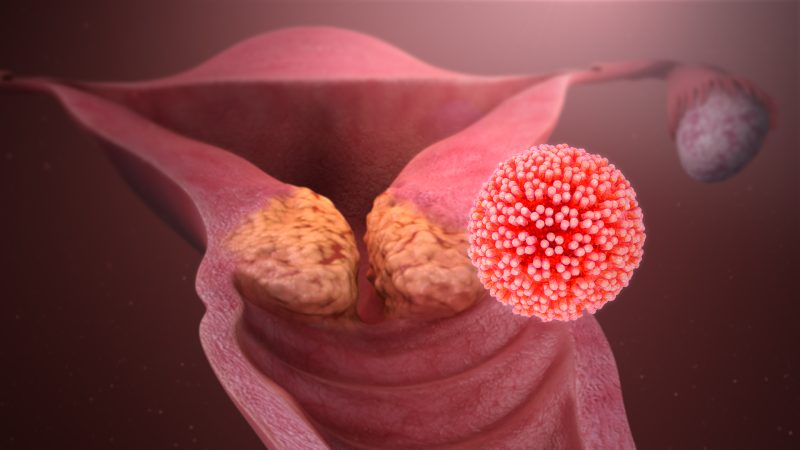
The end portion of the uterus where it meets the vagina is called the cervix. A malignant tumor of the cervix is called cervical cancer. Cervical cancer is the 3rd most common gynecological cancer which is more prevalent in developing countries. The average age of diagnosis is 52.
The outer part of the portion of cervix that protrudes into the vagina is called the ectocervix and the inner part is called the endocervix. Between the ecto and endo cervix is the transformation zone. Most of the cancer arises in this zone.
There are two types of cervical cancer. Squamous cell carcinoma accounts for 80-95% of all cervical cancer and is generally seen in older women. Adenocarcinoma accounts for 5-10% of all cervical cancer and is common in younger patients.
Symptoms
Cervical cancer is asymptomatic in the early stages of the disease. As the disease grows more and more symptoms arise. The most common symptom is vaginal discharge. The discharge starts as watery and starts to turn red and then brown in time. The discharge has a very strong odour. The most common symptom in post-menopausal patients is abnormal vaginal bleeding. Post-coital bleeding can also be a symptom of cervical cancer. Post-coital becomes more frequent as the severity of the disease grows. Patients also complain about vaginal pain and discomfort, and continuous pelvic and back pain. Painful and uncomfortable urination is also a symptom of this disease. Other complications of this disease include constipation, urinary obstruction, haematuria, pain, leg edema and hydronephrosis.
Causes
HPV stands for human papillomavirus, a non-enveloped double-stranded DNA virus, and is the major cause of cervical cancer. There are around 100 types of HPV. While type 16 and type 18 have high chances, type 6 and type 11 have the least chances of giving cervical cancer. While a one-time infection does not cause cervical cancer, repeated infection increases the chance of the disease. HPV infects cells of the stratum basale. Infected cells differentiate into squamous epithelial cells. HPV releases E6 and E7 proteins that inhibit p53 and Rb proteins in the cells. Rb and p53 proteins are tumor suppressors and are called cell division checkpoints. The inhibition leads to more cellular proliferation. This leads to dysplasia which is the uncontrolled growth of abnormal cells. This in turn increases the risk of cervical cancer. There are various risk factors for cervical cancer which include repeated HPV infection. HIV infection increases the chance of cervical cancer by five-fold. Smoking is also a risk factor as it suppresses the immune system. Vitamin deficiency and malnutrition is also a risk factor. Immunosuppressants such as AIDS and diabetes increase the risk of cervical cancer. If a first-degree family member has cervical cancer, the chances of cervical cancer increase due to genetic predisposition.
Treatment
There are three options for treatment- surgery, radiation therapy and chemotherapy. The patient may receive one or a combination of these treatments depending on the size of the tumor.
The surgical procedure depends upon the stage of cancer and whether the patient wants to have children later in life. In the early stage I the surgical oncology doctor may perform conization which is the removal of a cone-shaped piece of the cervix. Leap or loop electrosurgical excision is a conization procedure where a thin wire heated by electricity is used to remove the tissue. In the later stage IA and IB the surgeon may perform a radical trachelectomy in which most of the cervix and upper part of the vagina is removed but the uterus is preserved so it can be possible to have children. The surgeon places a stitch at the lower end of the uterus to act as an artificial internal opening of the cervix. During early-stage IA the surgeon may perform a total hysterectomy which is the removal of the uterus and cervix. During later stages 1A and 1B the surgeon may perform a radical hysterectomy removing the cervix, the tissue around the cervix, the uterus and part of the vagina. Other tissues such as the fallopian tubes, ovaries or lymph nodes may also be removed if necessary. If cancer has recurred the surgeon may perform pelvic exaggeration. In this procedure the pelvic lymph nodes, bladder, vagina, rectum and colon may have to be removed in addition to a radical hysterectomy depending on where the cancer has spread.
Radiation therapy or radiotherapy uses high-energy rays to kill cancer cells. There are two types of radiation therapy – External beam radiation (EBRT) and Brachytherapy. External beam radiation is a procedure in which X-rays are directed toward cancer from a machine from outside the body. It is similar to taking a normal x-ray but the intensity of the beam is stronger. It is taken multiple times and is usually coupled with chemotherapy. Brachytherapy is internal radiation therapy directed at the location of cancer from a device placed inside your body.
Chemotherapy is the use of anti-cancer drugs which are administered through the mouth or directly injected into the vein and hence enter the bloodstream. Chemotherapy can be used when the cancer has spread to other organs as well.
In India, one can consider looking for cancer treatment in Kerala as the state provides cost-effective treatments.


















